The Leadership Formula: Lessons from the Mayo Clinic
Exploring how intentional leadership development and organizational structure fuel world-class healthcare.
This blog is based on topics covered in Episode 3: Leadership by Design at the Mayo Clinic with Dr. Stephen Swensen and my site visit to the Mayo Clinic.
If you haven’t listened to it yet, check it out on Apple, Spotify, Substack or wherever you get your podcasts.
What can be learned from a Healthcare System that embedded leadership from the start?
Tell The Story.
When learning about the Mayo Clinic, you can’t go past its remarkable history. Its origins are in the 1880s when a family of doctors (the Mayo’s) and an order of local Nuns created the first clinic1. Fast forward 150 years, and it has grown into a globally renowned 17 billion dollar non-profit healthcare system and is consistently rated as the number one hospital in the US by US News2.
Not only is it a fascinating story from humble beginnings - but it’s an integral part of the Mayo Clinic’s identity. Spend any time in the small town of Rochester, Minnesota and you can’t go past its deep-rooted connection to the Clinic.
Everywhere you look, be it historic Mayo buildings, statues, museums, city tours and even in hospital merch shop - you’re reminded of the inedible mark this healthcare system has left on the town. When talking to staff about leadership, clear themes of legacy shone through.
So why does this matter?
On the path to excellence, having a clear, consistent and compelling story for a healthcare entity creates a shared identity and purpose. This unity allows for intangible but vital acts of goodwill and discretionary effort that only come from being connected to the story.
It also offers an important reflection point for healthcare systems to recognise their accountability and responsibility to everyone in the community. For some, this will be an opportunity to reconcile with the past, build bridges with the present, and co-create the future.
Healthcare is more than just the four walls of great buildings - it is the story (good and bad) of how its impacts ripple across communities and generations.
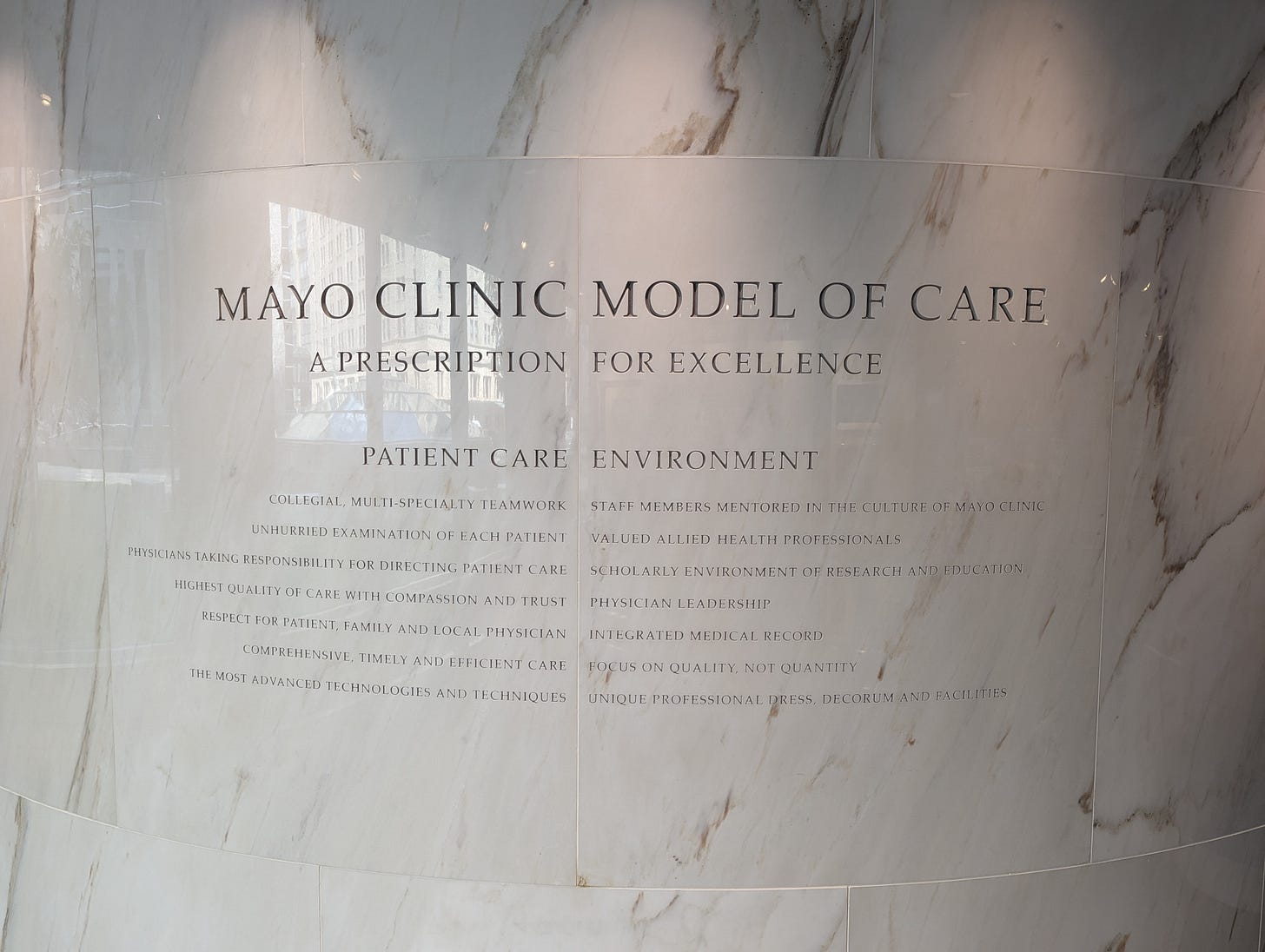
Build The Foundation.
From the beginning, the Mayo Clinic has prided itself on being a physician-led organisation. It is the belief that physicians should be in leadership roles due to their unique relationship with providing care.
To live up to this promise they’ve had to create a well-crafted structure for physicians. This includes a focus on a dyadic model of a physician and administrator partnership.
Several structures and processes ensure a carefully selected talent pool, rigorous onboarding, annual surveys, robust clinical committees and quality improvement programs34. These are all buttressed by a democratic internal voting system, established term limits for leadership roles and transparent compensation structures.
While organisational structure does not solve everything, they do lay a foundation and direction of travel. For example; the logo of the Mayo Clinic (the three shields) reflects the three priorities of physicians, clinical practice, education and research.
This intentional investment and engagement with the workforce is a strong value proposition to draw in and retain talent. Done right, these can become the guardrails to ensure the mission and values of the organisation are maintained, regardless of who is in leadership.
Listen And Learn.
A core tenet of the Mayo Clinic’s approach is the creation of feedback mechanisms. This means comprehensive surveying of staff and patients to ensure they both get to share their experiences. These results are quantified, analysed and followed up on with necessary development opportunities.
Through this process, they found that meaningful improvements in leadership metrics can result in improvement in staff satisfaction and a decrease in physician burnout5.
Your workforce is like the immune system to the organisational body. Ensuring multiple swift two-way communication channels can allow the body and immune system to appropriately communicate and respond (or appropriately not respond) to threats.
This has to be with the intention of finding out things you don’t know and not just a tick-box exercise. Staff are discerning and quickly disengage if feedback channels are not properly managed. From an organisational standpoint, if you don’t want to know what your immune system is telling you - you’re in trouble.
An equally important part is then acting on this information. This includes transparency of results and co-creating priorities and actions.
A Broader Definition of Leadership.
From my experience at various healthcare systems in the US, it has become evident that no single healthcare system is exempt from the mounting challenges.
However, those who recognise a values-based, collective, and multidisciplinary leadership lens, offer a compelling way forward.
For me, I think in this time of volatility and uncertainty, doubling down on improving the experience of frontline staff is vital. From my small sample at the Mayo Clinic, just having enough time to fulfil all of the lofty goals can be a challenge.
This also includes asking hard, introspective questions of leaders and organisations, to ensure they are value-aligned with the workforce and their community.
Finally, if COVID-19 has taught us anything, it’s that in our interconnected world, our collective safety is intrinsically tied to the well-being of the most vulnerable. This asks us to extend our leadership remit beyond the confines of our organisation to our broader society.
https://circulatingnow.nlm.nih.gov/2016/06/14/the-origins-and-evolution-of-the-mayo-clinic/
https://health.usnews.com/best-hospitals/area/mn/mayo-clinic-6610451
McCarthy, D, Mueller, K, Wrenn, J. (2009 “Mayo Clinic: Multidisciplinary Teamwork, Physician-Led Governance, and Patient-Centered Culture Drive World-Class Health Care”. Found at: https://collections.nlm.nih.gov/catalog/nlm:nlmuid-101537958-pdf
Swensen, S., Gorringe, G., Caviness, J. and Peters, D. (2016), "Leadership by design: intentional organization development of physician leaders", Journal of Management Development, Vol. 35 No. 4, pp. 549-570. https://doi.org/10.1108/JMD-08-2014-0080
Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, West CP. “Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014.” Mayo Clin Proc. 2015 Dec;90(12):1600-13. doi: 10.1016/j.mayocp.2015.08.023.